What Is The Differential Diagnosis Of Sjs/ten
In the differential diagnosis of SJS/TEN consider:
- Other severe cutaneous adverse reactions to drugs
For further details, see Stevens Johnson syndrome / toxic epidermal necrolysis: nursing management.
Care of a patient with SJS/TEN requires:
- Cessation of suspected causative drug the patient is less likely to die, and complications are less if the culprit drug is on or before the day that blisters/erosions appear
- Hospital admission preferably immediately to an intensive care and burns unit with specialist nursing care, as this improves survival, reduces infection and shortens hospital stay
- Consider fluidised air bed
- Nutritional and fluid replacement by intravenous and nasogastric routes reviewed and adjusted daily
- Temperature maintenance as body temperature regulation is impaired, the patient should be in a warm room
- Pain relief as pain can be extreme
- Sterile handling and reverse isolation procedures.
Skin care
- Examine daily for the extent of detachment and infection .
- Topical antiseptics can be used
- Dressings such as gauze with petrolatum, non-adherent nanocrystalline-containing silver gauze or biosynthetic skin substitutes such as Biobrane® can reduce pain.
- Avoid using adhesive tapes and unnecessary removal of dead skin leave the blister roof as a biological dressing.
Eye care
- Daily assessment by an ophthalmologist
- Frequent eye drops/ointments
Mouth care
- If ulcerated, prevent vaginal adhesions using intravaginal steroid ointment, soft vaginal dilators.
General
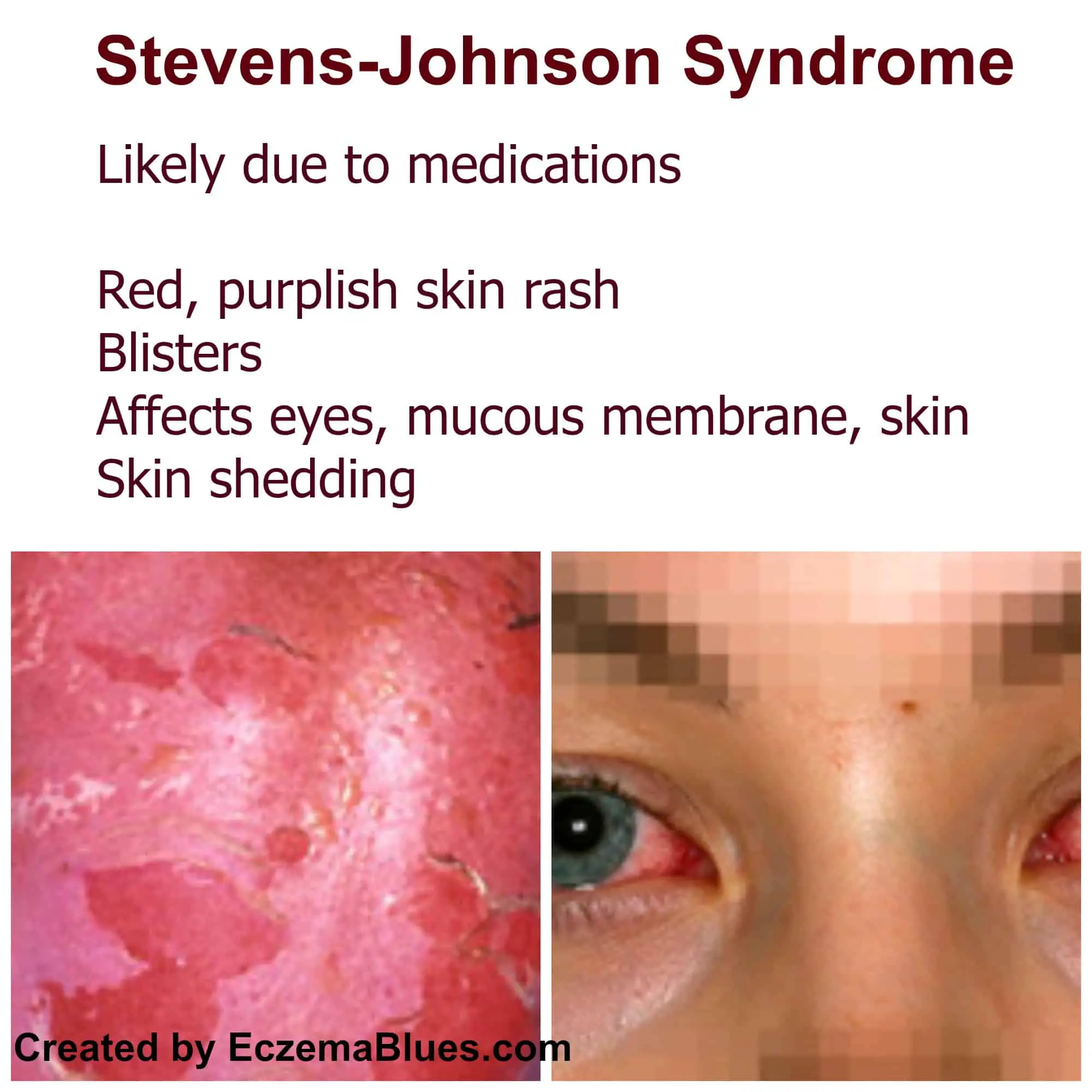
What Are The Signs And Symptoms Of Sjs
You may have a fever and chills up to 2 weeks before you have skin symptoms. You may also have a cough and sore throat, headache and body aches, and feel more tired than usual. Skin symptoms include the following:
- Sores that look like targets
- Painful mouth sores that make it hard to swallow or breathe
- Painful blisters on your skin, eyes, or genitals
- Sunburned appearing skin once the top layer falls off
Time To Onset Of Vancomycin
We describe the time to onset of vancomycin and linezolid in Figure 1. The median time to onset of linezolid-related SJS was 5 days , significantly earlier than vancomycin-related SJS . In general, vancomycin and linezolid-induced SJS had a higher onset time overall, while vancomycin and linezolid were special-use antibacterial drugs and should not be used for a long time. During use, more attention should be paid to monitoring adverse reactions at the initial stage of medication, especially linezolid.
FIGURE 1. The onset time of vancomycin- and linezolid-associated SJS.
Also Check: Buy Antibiotics For Bv Online
What Are The Signs And Symptoms Of Stevens
Before the skin symptoms start, many people report feeling generally unwell with a headache and joint pain, accompanied by a cough.
The main feature of Stevens-Johnson syndrome is a skin rash. The affected patches may look like a target with a purple or dark area of skin surrounded by a lighter area. Initially, the skin may be discoloured but then blisters develop which burst and leave sore areas. The rash is not usually itchy. Crops of discoloured areas may develop over a period of several weeks.
The mucous membranes moist areas of tissue such as the eye, inside of the mouth and throat are also affected with blisters and ulceration. Ulceration of the mucous membranes has the potential to cause the most serious problems such as dehydration because swallowing is so painful. Heat loss can also occur if large areas of skin are damaged. If the surface of the eye is affected, this could lead to long term damage if not treated promptly.
Who Is At Higher Risk

You’re more likely to get Stevens-Johnson syndrome if:
- you’ve had it before after taking a certain medicine you’re more likely to get it again if you take that medicine again or other similar medicines
- you have a weakened immune system for example, from having a condition like HIV or AIDS, or treatments like chemotherapy
- a close family member has had Stevens-Johnson syndrome sometimes your genes can mean you’re at higher risk of getting it
Don’t Miss: Are There Over The Counter Antibiotics For Strep Throat
What Is The Outlook For People Who Have Stevens
Each persons experience with Stevens-Johnson syndrome can be different. Skin can regrow in a matter of weeks, but recovery can take months if symptoms are severe. Some long-term reactions may develop, including:
- Skin: dryness, itching, change in skin color.
- Eyes: chronic swelling and/or dryness, chronic irritation, difficulty seeing, sensitivity to light .
- Excessive sweating.
Adverse Event And Drug Identification
We investigated adverse events by using the MedDRA Preferred Terms as follows: epidermal necrosis , epidermal necrolysis , SJS , toxic epidermal necrolysis , Stevens Johnson reaction . Therefore, MICROMEDEX ® was used like a dictionary. In addition, the trade names and common names of vancomycin and linezolid in the drug archives will also be listed.
Recommended Reading: How To Treat Uti At Home Without Antibiotics
What Medicines May Be Used To Treat Sjs
The goal of treating SJS is to stop symptoms from getting worse. You are put in the hospital to treat SJS. Your healthcare provider will stop the medicine you were taking that caused SJS. You may need any of the following:
- Antacids may be needed if sores grow in your stomach and cause bleeding.
- Antibiotics may be given to help treat an infection in your blood. Antibiotics may also be put on your skin to lower your risk for infection.
- Blood thinners help stop clots from forming in your blood if you are not able to get out of bed.
- Eye drops may be used to help eye sores heal and to prevent infection.
- Pain medicines help take away or decrease your pain.
- Immune globulins may be given to make your immune system stronger. You may need immune globulins to treat or prevent an infection.
- Pressors may be given to increase your blood pressure. A normal blood pressure helps protect your heart, lungs, brain, kidneys, and other organs.
Associations Between Stevensjohnson Syndrome And Infection: Overview Of Pharmacoepidemiological Studies
- 1Division of Cohort Research, Center for Public Health Sciences, National Cancer Center, Tokyo, Japan
- 2Division of Medicinal Safety Science, National Institute of Health Sciences, Kanagawa, Japan
StevensJohnson syndrome and toxic epidermal necrolysis are classified as type B adverse drug reactions, and are severe, potentially fatal rare disorders. However, the pathogenesis of SJS/TEN is not fully understood. The onset of SJS/TEN is triggered by the immune system in response to antigens with or by drugs. As activation of the immune system is important, infection could be a risk factor for the onset of SJS/TEN. Based on the hypothesis that infections induce the onset of SJS/TEN, we conducted pharmacoepidemiological investigations using two spontaneous adverse drug reaction reporting databases and Japanese medical information database. These data suggest that infection could be a risk factor for the development of SJS/TEN. In this mini-review, we discuss the association between infection and the development of SJS/TEN.
Also Check: Can Your Doctor Prescribe Antibiotics Over The Phone
Which Drugs Are Most Associated With Stevens
New findings from a study published in the American Journal of Medicine may help clinicians identify high-risk drugs and high-risk patients linked to the development of Stevens-Johnson syndrome /toxic epidermal necrolysis in order to reduce its incidence.
Mortality rates for SJS have been reported between 15% and 2535% for patients with TEN. Research has suggested that early recognition and prompt withdrawal of the implicating drug can lead to higher rate of patient survival.
To identify the drugs most associated with triggering SJS or TEN, researchers from Canada conducted a retrospective chart review on patients admitted to Vancouver General Hospital for SJS or TEN from 20012011. They also aimed to establish the timeline of identifying and removing these triggers as well as differences in mortality and drug exposure between ethnicities.
In 75% of the evaluated cases, a trigger was identified. Thirteen cases involved patients taking multiple drugs , which made it hard to isolate a single culprit drug. The single most common drug was allopurinol, which was responsible for 20% of the cases. Other common triggers were anticonvulsants and antibiotics .
The implicated drug was often removed at the time of admission or at the time of diagnosis, about 4-5 days after onset of symptoms. Researchers noted that the causative agent was discontinued at the onset of symptoms in only 19% of cases.
Prognosis For Sjs And Ten
Severe toxic epidermal necrolysis is similar to extensive burns patients are acutely ill, may be unable to eat or open their eyes, and suffer massive fluid and electrolyte losses. They are at high risk of infection, multiorgan failure, and death. With early therapy, survival rates approach 90%. The severity-of-illness score for toxic epidermal necrolysis Severity-of-Illness Score for Toxic Epidermal Necrolysis systematically scores 7 independent risk factors within the first 24 hours of presentation to the hospital to determine the mortality rate for a particular patient.
The TNF-alpha inhibitors infliximab and etanercept can help reduce inflammation.
Thalidomide has also been tested but increases mortality and is now contraindicated.
Recommended Reading: Can I Get Dog Antibiotics Over The Counter
Working On A Manuscript
| Medical records were used to validate the diagnosis and culprit drug/s of each StevensJohnson syndrome/toxic epidermal necrolysis case that occurred, in a community-based unselected cohort of 4.7 million patients between 2008 and 2019. |
| Cumulative incidence of StevensJohnson syndrome/toxic epidermal necrolysis was calculated for each drug, based on the total number of new users in the community. |
Diagnosis Of Sjs And Ten
-
Clinical evaluation
-
Often skin biopsy
Diagnosis is often obvious from appearance of lesions and rapid progression of symptoms. Histologic examination of sloughed skin shows necrotic epithelium, a distinguishing feature.
. Characteristics of staphylococcal scalded skin syndrome usually include sparing of mucous membranes, absence of risk factors for TEN , and clinical suspicion of staphylococcal infection.
Recommended Reading: Antibiotic Eye Cream For Cats
How Goldenberglaw Can Help You
If you, or a loved one, has been diagnosed with Stevens-Johnson Syndrome while taking a medication listed above, you may have a case against the clinic or pharmacy due to a failure to warn or wrongful dosing of the medication. the Stevens-Johnson Syndrome attorneys at GoldenbergLaw today for a free consultation. We understand the devastating effects of SJS. Our team of Stevens-Johnson Syndrome lawyers have the experience and expertise needed to bring a complex malpractice claim. We have over 30+ years of experience holding negligent medical providers accountable. Leave the sleepless nights to us.
Pathophysiology Of Sjs And Ten
The exact mechanism of Stevens-Johnson syndrome and toxic epidermal necrolysis is unknown however, one theory holds that altered drug metabolism in some patients triggers a T-cellmediated cytotoxic reaction to drug antigens in keratinocytes. CD8+ T cells have been identified as important mediators of blister formation.
Findings suggest that granulysin released from cytotoxic T cells and natural killer cells might play a role in keratinocyte death granulysin concentration in blister fluid correlates with severity of disease. Interleukin-15 has also been found to be increased in patients with SJS/TEN and has been found to increase granulysin production. Another theory is that interactions between Fas and its ligand, particularly a soluble form of Fas ligand released from mononuclear cells, lead to cell death and blister formation. A genetic predisposition for SJS/TEN has been suggested.
Also Check: What Antibiotic For Staph Infection
When To Get Medical Help
SJS must be treated immediately.
Although early symptoms usually resemble that of a flu, you should seek medical help right away if you also meet any of the following criteria:
- started taking new medication in the last 8 weeks
- have a rash that you believe may be SJS
- have a family history of SJS or TEN
- have a previous diagnosis of SJS or TEN
There is no specific test or criteria to diagnose SJS.
A doctor, often a specialist like a dermatologist, will diagnose your condition based on your medical history and the symptoms youre experiencing.
Doctors may take a skin sample, called a biopsy, or perform other diagnostic tests to help confirm SJS and rule out other conditions.
Pearls And Other Issues
Death is mainly due to sepsis and multiorgan failure. Contributing causes are:
- Gastrointestinal bleeding
- Pulmonary embolism
- Myocardial infarction and pulmonary edema
People who have survived Stevens-Johnson syndrome/toxic epidermal necrolysis must avoid the causative drug or structurally related medicines as Stevens-Johnson syndrome/toxic epidermal necrolysis may recur. Cross-reactions can occur between:
- Anticonvulsants carbamazepine, phenytoin, lamotrigine and phenobarbital
- Beta-lactam antibiotics penicillin, cephalosporin, and carbapenem
- Nonsteroidal anti-inflammatory drugs
- Sulfonamides sulfamethoxazole, sulfadiazine, sulfapyridine
Stevens-Johnson syndrome/toxic epidermal necrolysis survivors may have scarring. Severe consequences can include:
- Ocular sequelae: dry eye, photophobia, pain, symblepharon, corneal scarring or neovascularization, trichiasis, reduced visual acuity, and blindness
- Cutaneous scarring, depigmentation, development of new melanocytic nevi, and pruritus
- Nail dystrophy, onycholysis, and loss of nails
- Diffuse scalp hair thinning
- Vulvovaginal stenosis or occlusion in females and phimosis in males
- Persistent pulmonary disease: bronchitis, bronchiectasis, bronchiolitis obliterans, organizing pneumonia, respiratory tract obstruction
Don’t Miss: Do You Always Need Antibiotics For Sinus Infection
What Treatments May Be Used For Sjs
- Wound care is done to protect skin sores and help them heal.
- Hydrotherapy is done in a whirlpool to help clean your wounds, and to remove dead tissue from your skin.
- Physical therapy may be needed to help your arm and leg movement if you have to stay in bed.
- Surgery may be needed if your skin does not heal properly. You may need debridement to clean the wounds and to remove dirt or dead tissues. A skin graft may be done to cover and help heal the areas where you lost skin.
- TPN is liquid nutrition that provides your body with protein, sugar, vitamins, minerals, and sometimes fat . TPN is used when you have problems with eating or digesting food.
Symptoms And Signs Of Sjs And Ten
Within 1 to 3 weeks after the start of the offending drug, patients develop a prodrome of malaise, fever, headache, cough, and keratoconjunctivitis. Macules, often in a target configuration, then appear suddenly, usually on the face, neck, and upper trunk. These macules simultaneously appear elsewhere on the body, coalesce into large flaccid bullae, and slough over a period of 1 to 3 days. Nails and eyebrows may be lost along with epithelium. The palms and soles may be involved. Skin, mucosal, and eye pain are common. In some cases, diffuse erythema is the first skin abnormality of toxic epidermal necrolysis.
In severe cases of toxic epidermal necrolysis, large sheets of epithelium slide off the entire body at pressure points , exposing weepy, painful, and erythematous skin. Painful oral crusts and erosions, keratoconjunctivitis, and genital problems accompany skin sloughing in up to 90% of cases. Bronchial epithelium may also slough, causing cough, dyspnea, pneumonia, pulmonary edema, and hypoxemia. Glomerulonephritis and hepatitis may develop.
Don’t Miss: How Much Does An Antibiotic Cost
Are There Other Names For Stevens
Yes. It is also known as Lyells syndrome, Stevens-Johnson syndrome/toxic epidermal necrolysis, and Stevens-Johnson syndrome toxic epidermal necrolysis spectrum. It might be called drug-induced Stevens-Johnson syndrome or mycoplasma-induced Stevens-Johnson syndrome if its linked to a specific cause.
How Is Sjs/ten Diagnosed

SJS/TEN is suspected clinically and classified based on the skin surface area detached at maximum extent.
- Skin detachment < 10% of body surface area
- Widespreaderythematous or purpuric macules or at atypical targets
Overlap SJS/TEN
- Detachment between 10% and 30% of BSA
- Widespread purpuric macules or at atypical targets
TEN with spots
- Widespread purpuric macules or at atypical targets
TEN without spots
- Detachment of > 10% of BSA
- Large epidermal sheets and no purpuric macules
The category cannot always be defined with certainty on initial presentation. The diagnosis may, therefore, change during the first few days in the hospital.
Don’t Miss: Can You Get Antibiotics Over The Phone
Results Of A Pharmacoepidemiological Study Using The Jader Database
First, to elucidate the association between infection and SJS/TEN, we conducted a pharmacoepidemiological study using the JADER database .
JADER is a large published spontaneous reporting database for drug adverse reactions that was established by Japan’s Pharmaceuticals and Medical Device Agency for pharmacovigilance activities. The dataset can be accessed directly on: , and compose of four relational tables: DEMO, DRUG, REAC, and HIST. The tables contain the following information: demographic information of patients including, sex and age , drug information used in patients , adverse drug information that have occurred in patients and primary disease information . Each table was connected using the ID number of each recorded case.
Late Phase And Sequelae
Sequelae are common features of late phase TEN. According to the study of Magina et al following symptoms are found: hyper- and hypopigmentation of the skin , nail dystrophies , and ocular complications. According to a study of Yip et al. 50% of patients with TEN develop late ocular complications including, by order of decreasing frequency, severe dry eyes , trichiasis , symblepharon , distichiasis , visual loss , entropion , ankyloblepharon , lagophthalmos , and corneal ulceration . Hypertrophic scars are only seen in very few patients . Long-term complications of mucosal involvement occur in 73% of patients who present mucosal involvement in the acute phase, and the mucosal sequelae involve mainly the oral and oesophageal mucosa, and to a lesser extent lung and genital mucosa . In a small post SJS/TEN study seven out of nine patients had either xerostomia or keratoconjunctivitis or both, resembling Sjögren-like syndrome . Additionally, another group reported a patient with Sjögren-like pluriglandular exocrine insufficiency including exocrine pancreatic impairment .
Recommended Reading: What Antibiotic Should You Take For A Sinus Infection
Enhancing Healthcare Team Outcomes
The management of SJS is interprofessional. A number of specialists are usually involved in the care of these patients, including a dermatologist, intensivist, ophthalmologist, pulmonologist, nephrologist, plastic surgeon, and gastroenterologist, functioning as an interprofessional team. The acute care of these patients is provided by wound care. The pharmacist must also closely assess the medications that the patient is receiving to prevent exacerbation of the disorder or determine if any of the patient’s medications could be the trigger for the condition. Even after treatment, these patients may have severe cosmetic deficits and may require mental health counseling. If the lesions occur across joints, the patient may benefit from physical therapy to restore function and muscle strength. The patient has to be educated on the use of ocular lubricants because of the sicca-like syndrome. Many patients do lose weight after suffering a severe reaction and should be referred to a dietitian. Following discharge, the patients need long-term follow-up to ensure that there are no functional deficits, including vision loss. Once a patient has suffered an SJS, it is highly recommended that the patient wear a warning bracelet indicating the toxic agent or allergen.
Outcomes